Next: Emphasized conditions Up: Course activities Previous: Office preceptorship
At your office sessions, most of you will eventually be writing notes in the charts of the patients you see. Each preceptor has a different way of handling this, because the documentation systems in the offices vary greatly. And each of you will progress in your charting skills at different rates. Presumably your preceptor will give you feedback along the way.
It would also be useful for me to see samples of your work. Hopefully I can provide some useful feedback to you as well. Thus, at each half-day session of office hours, you should prepare a brief SOAP note on one of the patients you saw that day, and then submit it on Blackboard. This is something that you should prepare and submit that very afternoon on the fly. Don't put it off beyond that very same evening. It is nothing that should require research in the library or anything that intense. The notes should in general be one page or less.
I will provide, also on Blackboard, brief comments on as many of your notes as I can. Questions that I pose in my comments are not rhetorical: please answer them, via the discussion board on Blackboard.
Notes should be submitted weekly, one at a time. Try to submit each note on the day you see the patient. If you keep up with this pattern, you will never need to submit a bunch together and in fact, I will not accept or review more than one at a time.
I have a number of educational goals in mind for the SOAP notes. There are two that speak directly to the issue of handing them in regularly and not batched:
At the top of your note, you should indicate your degree of involvement in the encounter, as follows:
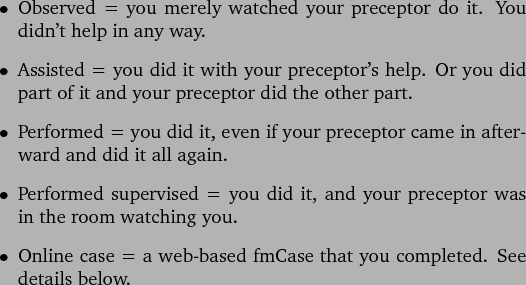
``Performed supervised'', though it doesn't sound as impressive as "performed", is an effective way to learn. As the year progresses and you get more comfortable on your own, please continue to avail yourself of the opportunity to have your preceptor watch you.
Also at the top of the note, you should indicate whether you, personally, have seen this patient before. Say ``yes'' only if you, the student, have personally seen this patient in the office before. For example, this item should obviously be ``no'' for the note you write on your first day at your office. ``Yes'' answers should become more frequent as the year progresses.
Please do not include any patient-identifying information: No name, initials, date seen, address, phone number, medical record number, social security number, birthdate, etc. Also, do not include your preceptor's name. The patient's age and sex are fine and should be included.
These notes will be visible to everyone in the class. This is so we can all read them, comment upon them, and learn from each other. Collaborative discussion of cases is one of the most powerful learning experiences in medicine. I encourage everyone to read each other's posted SOAP notes and then post questions and comments about them. As Deborah Meier says, ``Teaching is mostly listening and learning is mostly talking.'' (Or, in the computer era-typing!)
I track the reasons for visit and the diagnoses of the patients that you see by using alphanumeric codes from the second edition of the International Classification of Primary Care (ICPC-2). This is a coding scheme developed mainly under the auspices of the World Organization of Family Doctors. It is designed to be relevant to the sorts of problems seen in general practice. Each clinical problem is coded with a letter, indicating the general category, and a 2-digit number, indicating a more specific diagnosis. For example, hypertension is K86, (K for cardiovascular.) Any given encounter can entail an infinite number of diagnostic codes. You will see these codes on your SOAP notes, along with my comments about your notes, when you look back at them on Blackboard.
RMED students are done with their Binghamton-based primary Care weekly office hours upon departure from Binghamton in the spring. However, they will continue to see patients with the new RMED family physician preceptor, and they should continue uploading one SOAP note per week.
You will probably not see every patient on your preceptor's schedule each afternoon you are there. So you and your preceptor will exercise some judgment in choosing patients for you to see. Who you see each week is driven by a variety of factors; who you write up and submit is up to you. As you see patients and write notes each week, keep these points in mind, in roughly decreasing order of priority:
As always, you must work with your preceptor to meet the needs of your patients in the most effective and efficient manner possible.
Lastly, if you address multiple problems in a patient who you intend to write up and submit, be sure to document all the problems that you addressed.